A blog designed to help medical students and doctors preparing for undergraduate and postgraduate exams
Monday, November 27, 2017
Nausea And Weight Loss In A 45 Year old Alcoholic... Case Study
A 45 years old man consults his general practitioner (GP) with a 6-month history of reduced appetite
and a weight loss, from 78 to 71 kg. During the last 3 months he has had intermittent nausea, especially in the mornings, and in the last 3 months the morning nausea has been accompanied by vomiting on several occasions. For 1 month he has noted swelling of his ankles. Despite his weight loss he has recently noticed his trousers getting tighter. He has had no abdominal pain. He has no relevant past history and knows no family history as he was adopted.
He takes no medication. From the age of 18 he has smoked 5–6 cigarettes daily and drunk 15–20 units of alcohol per week. He has been a chef all his working life, without exception in fashionable restaurants. He now lives alone as his wife left him 1 year ago.
Examination
He has plethoric features. There is pitting oedema of his ankles. He appears to have lost weight from his limbs, but not his trunk. He has nine spider naevi on his upper trunk.
His pulse is normal, and the rate is 92/min. His jugular venous pressure (JVP) is not raised, and his blood pressure is 146/84 mmHg.
The cardiovascular and respiratory systems are normal.
The abdomen is distended. He has no palpable masses, but there is shifting dullness and a fluid thrill
Investigations:
Haemoglobin = 12.6 g/dL (normal = 13.3–17.7 g/dL)
White cell count = 10.2 × 109/L (normal = 3.9–10.6 × 109/L)
Platelets = 121 × 109/L (normal = 150–440 × 109/L)
Sodium = 131 mmol/L (normal = 135–145 mmol/L)
Potassium = 4.2 mmol/L(normal = 3.5–5.0 mmol/L)
Urea = 2.2 mmol/L (normal = 2.5–6.7 mmol/L)
Creatinine = 101 μmol/L (normal = 70–120 μmol/L)
Total protein = 48 g/L (normal = 60–80 g/L)
Albumin = 26 g/L (normal = 35–50 g/L)
Bilirubin = 25 mmol/L (normal = 3–17 mmol/L)
Alanine transaminase = 276 IU/L (normal = 5–35 IU/L)
Gamma-glutamyl transaminase = 873 IU/L (normal = 11–51 IU/L)
Alkaline phosphatase = 351 IU/L (normal = 30–300 IU/L)
International normalised ratio (INR) = 1.4 (normal = 0.9–1.2)
Urinalysis: no protein; no blood
• What is the diagnosis?
• How would you manage this patient?
Thursday, September 28, 2017
Regarding Rotator Cuff Injury...
A 23-year-old man presents following a fall onto his left shoulder whilst playing rugby. He complains of pain throughout the shoulder and on examination has weakness when testing internal rotation of the arm compared to the contralateral side.
Radiographs are negative.
Injury to which tendon would explain his symptoms?
A Deltoid
B Infraspinatus
C Subscapularis
D Supraspinatus
E Teres minor
Answer:
A first-time mother brings in her 5-day-old baby for a well-child visit....
A first-time mother brings in her 5-day-old baby for a well-child visit. The nurse weighs the infant and reports a weight of 7 lb 5 oz to the mother. The mother looks concerned and tells the nurse that her baby weighed 7 lb 10 oz when she was discharged 4 days ago.
The nurse’s best response to the mother is:
A. “I will let the doctor know, and he will talk with you about possible causes of your infant’s weight loss.”
B. “A weight loss of a few ounces is common among newborns, especially for breastfeeding mothers.”
C. “I can tell you are a first-time mother. Don’t worry; we will find out why she is losing weight.”
D. “Maybe she isn’t getting enough milk. How often are you breastfeeding her?”
Answer:
Wednesday, September 27, 2017
A 40 Year old patient presenting with nausea, vomiting and abnormal liver function tests...
A 40-year-old school teacher develops nausea and vomiting at the beginning of the fall semester. Over the summer she had taught preschool children in a small town in Mexico. She is sexually active, but has not used intravenous drugs and has not received blood products.
Physical examination reveals scleral icterus, right upper quadrant tenderness, and a palpable liver. Liver function tests show aspartate aminotransferase of 750 U/L (normal < 40) and alanineaminotransferase of 1020 U/L (normal < 45). The bilirubin is 13 mg/dL (normal < 1.4) and the alkaline phosphatase is normal.
What further diagnostic test is most likely to be helpful?
a. Liver biopsy
b. Abdominal ultrasound
c. IgM antibody to hepatitis A
d. Antibody to hepatitis B surface antigen
e. Determination of hepatitis C RNA
Answer:
Monday, September 25, 2017
Aortic Regurgitation - History, Examination And Study Questions & Answers
Clinical History
· Patients may be asymptomatic (but may have normal or depressed left ventricular function).
· Dyspnoea and fatigue (due to left ventricular impairment and low cardiac output initially on exertion).
· Symptoms of left ventricular failure in later stages.
· Angina pectoris is less common than in aortic stenosis; it usually indicates coronary artery disease.
Examination
1. Pulse
· Collapsing pulse (large volume, rapid fall with low diastolic pressure).
· Visible carotid pulsation in neck (dancing carotids or Corrigan's sign).
· Symptoms of left ventricular failure in later stages.
· Angina pectoris is less common than in aortic stenosis; it usually indicates coronary artery disease.
Examination
1. Pulse
· Collapsing pulse (large volume, rapid fall with low diastolic pressure).
· Visible carotid pulsation in neck (dancing carotids or Corrigan's sign).
· Capillary pulsation in fingernails (Quincke's sign).
· A booming sound heard over femorals ('pistol-shot' femorals or Traube's sign).
· To and fro systolic and diastolic murmur produced by compression of femorals by stethoscope
(Duroziez's sign or murmur).
2. Heart
· Heart sounds are usually normal.
· Apex beat is displaced outwards and is forceful.
· Third heart sound (in early systole with bicuspid aortic valve).
· Early diastolic, high-pitched murmur is heard at the left sternal edge with the diaphragm - if not
readily apparent, it is important to sit the patient forward and auscultate with the patient's breath held
at the end of expiration. When the ascending aorta is dilated and displaced to the right, the murmur
may be heard along the right sternal border as well.
· An ejection systolic murmur may be heard at the base of the heart in severe aortic regurgitation
(without aortic stenosis). This murmur may be as loud as grade 5 or 6, and underlying organic stenosis can be ruled out only by investigations.
· Ejection click suggests underlying bicuspid aortic valve.
· Mid-diastolic murmur of Austin Flint may be heard at the apex. It is typically low-pitched, similar to the murmur of mitral stenosis but without a preceding opening snap.
· Loud pulmonary component of second sound (suggests pulmonary hypertension).
3. General examination
· Head nodding in time with the heart beat (de Musset's sign) may be present.
· Visible carotid pulsation may be obvious in the neck - dancing carotids or Corrigan's sign.
· Check the blood pressure (wide pulse pressure).
· Look for systolic pulsations of the uvula (Muller's sign).
· Check pupils for Argyll Robertson pupil of syphilis.
· Look for stigmata of Marfan's syndrome - high arched palate, arm span greater than height.
· Check joints for ankylosing spondylitis and rheumatoid arthritis.
· A booming sound heard over femorals ('pistol-shot' femorals or Traube's sign).
· To and fro systolic and diastolic murmur produced by compression of femorals by stethoscope
(Duroziez's sign or murmur).
2. Heart
· Heart sounds are usually normal.
· Apex beat is displaced outwards and is forceful.
· Third heart sound (in early systole with bicuspid aortic valve).
· Early diastolic, high-pitched murmur is heard at the left sternal edge with the diaphragm - if not
readily apparent, it is important to sit the patient forward and auscultate with the patient's breath held
at the end of expiration. When the ascending aorta is dilated and displaced to the right, the murmur
may be heard along the right sternal border as well.
· An ejection systolic murmur may be heard at the base of the heart in severe aortic regurgitation
(without aortic stenosis). This murmur may be as loud as grade 5 or 6, and underlying organic stenosis can be ruled out only by investigations.
· Ejection click suggests underlying bicuspid aortic valve.
· Mid-diastolic murmur of Austin Flint may be heard at the apex. It is typically low-pitched, similar to the murmur of mitral stenosis but without a preceding opening snap.
· Loud pulmonary component of second sound (suggests pulmonary hypertension).
3. General examination
· Head nodding in time with the heart beat (de Musset's sign) may be present.
· Visible carotid pulsation may be obvious in the neck - dancing carotids or Corrigan's sign.
· Check the blood pressure (wide pulse pressure).
· Look for systolic pulsations of the uvula (Muller's sign).
· Check pupils for Argyll Robertson pupil of syphilis.
· Look for stigmata of Marfan's syndrome - high arched palate, arm span greater than height.
· Check joints for ankylosing spondylitis and rheumatoid arthritis.
QUESTIONS
Splenomegaly - Case Study
This man presents with tiredness and lethargy. Please examine his abdominal system and discuss your
diagnosis.
Clinical signs To Look For:
General
• Anaemia
• Lymphadenopathy (axillae, cervical and inguinal areas)
• Purpura
Abdominal
• Left upper quadrant mass that moves inferomedially with respiration, has a notch, is dull to percussion and you cannot get above nor ballot
• Estimate size
• Check for hepatomegaly
Underlying cause
- Lymphadenopathy
- Haematological and Infective
- Stigmata of chronic liver disease
- Cirrhosis with portal hypertension
- Splinter haemorrhages, murmur, etc.
- Bacterial endocarditis
- Rheumatoid hands
- Felty’s syndrome
Discussion
Causes Of Splenomegaly
Causes Of Splenomegaly
Thursday, September 21, 2017
A 26-year-old G1P0 woman at 39 weeks’ gestation is admitted to the hospital in labor.
A 26-year-old G1P0 woman at 39 weeks’ gestation is admitted to the hospital in labor. She is noted to have uterine contractions every 7 to 10 minutes. Her antepartum history is significant for a nonimmune rubella status.
On examination, her blood pressure (BP) is 110/70 mm Hg and heart rate (HR) is 80 beats per minute
(bpm). The estimated fetal weight is 7 lbs.
On pelvic examination, she has been noted to have a change in cervical examinations from 4-cm dilation to 7 cm over the last 2 hours. The pelvis is assessed to be adequate on digital examination.
What is your next step in the management of this patient?
Next step in Management: Continue to observe the labor.
Learning Objectives In this Case
1. Know the normal labor parameters in the latent and active phase for nulliparous and multiparous patients.
2. Be familiar with the management of common labor abnormalities and know that normal labor does not require intervention.
3. Know that rubella vaccination, as a live-attenuated preparation, should not beadministered during pregnancy.
Case Discussion:
Sunday, July 30, 2017
A 24-year-old woman has acute renal failure following postpartum hemorrhage...
A 24-year-old woman has acute renal failure following postpartum hemorrhage. Laboratory studies showed
serum glucose, 150 mg/dL;
sodium, 135 mEq/L;
potassium, 6.5 mEq/L;
chloride, 105 mEq/L; and
bicarbonate, 15 mEq/L.
Therapy should include which of the following?
(A) Decrease potassium chloride to 10 mEq/L
(B) Intravenous 0.9% sodium chloride
(C) 100 mL of 50% glucose water with 10 U insulin
(D) Intravenous calcitonin
(E) Intravenous magnesium sulfate
Answer:
Regarding Child's Developmental Milestones...
A child is brought to your clinic for a routine examination. She can put on a T-shirt but requires a bit of help dressing otherwise. She can copy a circle well but has difficulty in copying a square. Her speech is understandable and she knows four colors. She balances proudly on each foot for 2 seconds but is unable to hold the stance for 5 seconds.
Which of the following is the most likely age of this child?
a. 1 year
b. 2 years
c. 3 years
d. 4 years
e. 5 years
Answer:
Which one of the following people should be offered the annual injectable influenza vaccine?
Which one of the following people should be offered the annual injectable influenza vaccine?
A. A 57-year-old man who had a stroke 15 years ago
B. A 55-year-old hypertensive man who has no complications from his condition
C. A 50-year-old woman with Crohn's disease
D. A 23-year-old man who has asthma. He describes his condition as 'mild' and only uses a salbutamol inhaler
E. A 51-year-old woman with hypothyroidism on thyroxine
Answer:
Friday, July 28, 2017
Diabetes In Pregnancy - Study Questions & Answers
A dilated ophthalmologic examination shows no retinopathy. An ECG is normal.
Urinalysis is negative for proteinuria.
Urinalysis is negative for proteinuria.
Laboratory studies show:
• HbA1c : 10.8%
• Glucose : 22 mg/dl
• TSH : 1.0 microU/ml
• Free thyroxine: 1.7 ng/dL
• Creatinine: 1.1 mg/dL.
Question: Which of the following condition has the same risk of developing in diabetics as the general population.
a. Asymptomatic bacteriuria
b. Preeclampsia
c. Congenital adrenal hyperplasia
d. PPH after delivery
e. Shoulder dystocia
Answer: c. Congenital adrenal hyperplasia
Question: A 30-yrs-old G3P2 patient visits an antenatal clinic at 20 weeks. She reveals during history that her first baby was 4.6 kg delivered by cesarean section, second baby was 4,8 kg delivered by c/section. Gynaecologists suspects gestational diabetes and orders a Glucose tolerance test. The blood sugar levels after 50 gms of oral glucose are 206 mg/dl and the patient is thus confirmed as a case of gestational diabetes.
Regarding the most common ECG finding of pulmonary embolism?
A 42-year-old man develops shortness of breath (SOB) and chest pain 7 days after an open cholecystectomy. His blood pressure is 145/86 mm Hg, pulse is 120/min, respiration 24/min, and oxygen saturation of 97%. Pulmonary embolism is clinically suspected.
Which of the following is the most common ECG finding of pulmonary embolism?
(A) a deep S wave in lead I
(B) depressed ST segments in leads I and II
(C) prominent Q wave in lead I, and inversion of T wave in lead III
(D) sinus tachycardia
(E) clockwise rotation in the precordial leads
Answer: (D) sinus tachycardia
Discussion: Sinus tachycardia is the most common ECG finding in pulmonary embolism.
The specific ECG signs of pulmonary embolism such as the S1, Q3, T3 are rarely seen except in cases of massive pulmonary embolism.
In submassive pulmonary emboli, the ECG may show nonspecific ST changes and sinus tachycardia.
On occasion, pulmonary embolism can precipitate atrial flutter or fibrillation.
Which of the following is the most common ECG finding of pulmonary embolism?
(A) a deep S wave in lead I
(B) depressed ST segments in leads I and II
(C) prominent Q wave in lead I, and inversion of T wave in lead III
(D) sinus tachycardia
(E) clockwise rotation in the precordial leads
Answer: (D) sinus tachycardia
Discussion: Sinus tachycardia is the most common ECG finding in pulmonary embolism.
The specific ECG signs of pulmonary embolism such as the S1, Q3, T3 are rarely seen except in cases of massive pulmonary embolism.
In submassive pulmonary emboli, the ECG may show nonspecific ST changes and sinus tachycardia.
On occasion, pulmonary embolism can precipitate atrial flutter or fibrillation.
Friday, July 21, 2017
Regarding Hypersensitivity Reactions...
A 20-year-old woman had her ears pierced when she was 16 years old. Since that time, she has had only two pairs of earrings, both given to her by her parents; both were 18 karat gold. Last week her
21-year-old boyfriend gave her a new pair of earrings for Valentine’s Day, which she started to wear immediately. Three days later, she developed localized areas of erythema and vesicle formation where she had pierced her ears.
The mechanism responsible for this reaction most closely resembles which of the following?
(A) Type I hypersensitivity
(B) An Arthus reaction
(C) A positive purified protein derivative (PPD) skin reaction
(D) Antibody-dependent cell-mediated cytotoxicity
(E) An immune complex disease
Answer:
Rates of successful pregnancy following three spontaneous losses (repeated miscarriages) are
Rates of successful pregnancy following three spontaneous losses (repeated miscarriages) are
a. Very poor
b. Slightly worse than those in the baseline population
c. No different from those in the baseline population
d. Just under 50%
e. Good unless cervical incompetence is diagnosed
Answer:
Thyrotoxicosis...
A 23-year-old woman presents with sweating and tremor. Her thyroid function tests are as follows:
- TSH <0.05 mU/l
- Free T4 25 pmol/l
What is the most common cause of this presentation?
A. Hashimoto's thyroiditis
B. Graves' disease
C. Toxic nodular goitre
D. De Quervain's thyroiditis
E. Toxic adenoma
Answer:
A 50-year-old patient presents with symptomatic nephrolithiasis. ..
A 50-year-old patient presents with symptomatic nephrolithiasis. He reports that he underwent a
jejunoileal bypass for morbid obesity when he was 39.
One would expect to find
a. Pseudohyperparathyroidism
b. Hyperuric aciduria
c. “Hungry bone” syndrome
d. Hyperoxaluria
e. Sporadic unicameral bone cysts
Answer:
Physiological changes in pregnancy: uterus and cervix - Extended matching question
Physiological changes in pregnancy: uterus and cervix - Extended matching question
A Oestradiol
B Prostaglandins
C Progesterone
D Cortisol
E Collagenase
F Prolactin
G Human chorionic gonadotrophin (HCG)
H Adrenocorticotrophic hormone (ACTH)
I Oxytocin
For each description below, choose the SINGLE most appropriate answer from the above list of options. Each option may be used once, more than once, or not at all.
1 Levels approximately 15 times higher in third trimester than in non-pregnant state.
2 Induces the process of cervical remodelling.
3 Regulates local uterine blood flow through endothelial effects.
4 Utilized in triple test.
5 Released from posterior pituitary gland.
Answers:
Thursday, July 20, 2017
A 68-year-old man has been very ill for months following the onset of chronic liver disease ...
A 68-year-old man has been very ill for months following the onset of chronic liver disease with hepatitis C infection. He experiences a sudden loss of consciousness and then exhibits hemiplegia on the right. A cerebral angiogram reveals lack of perfusion in the left middle cerebral artery distribution.
The most likely cardiac lesion to be associated with this finding is?
A- Acute rheumatic fever
B- Left atrial myxoma
C- Libman-Sacks endocarditis
D- Non-bacterial thrombotic endocarditis
E- Paradoxical thromboembolus
Answer:
Sunday, July 16, 2017
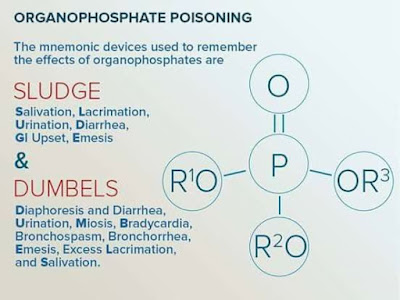
Which of the following statements is true concerning organophosphate poisoning?
Which of the following statements is true concerning organophosphate poisoning?
A. Their principal action is the stimulation of acetylcholinesterase activity
B. They are only absorbed through the respiratory tract
C. Miosis, sweating and hypersalivation are due to nicotinic-receptor effects
D. Atropine is useful in the management of organophosphate poisoning
E. Organophosphate neuropathy occurs within 24 hours
Answer:
Regarding anatomy of the heart...
Which of the following regarding the anatomy of the heart is true?
A) The aortic valve is tricuspid.
B) The ascending aorta is entirely outside the pericardial sac.
C) The left atrial appendage is identified readily by transthoracic echocardiography.
D) The pulmonary trunk lies anterior to the ascending aorta.
E) The right atrium is posterior to the left atrium.
Answer:
A 73-year-old man complains of right leg pain of 2 years’ duration...
A 73-year-old man complains of right leg pain of 2 years’ duration. There is no history of falls or injury. In the past he has been admitted to hospital for cardiac failure and takes inhaled bronchodilators and steroids for chronic obstructive pulmonary disease.
Examination shows a healthy elderly man with mild tenderness of his right leg only.
Routine blood tests show normal serum calcium and phosphate levels with a markedly raised alkaline phosphatase level.
What is the most likely diagnosis?
A. Osteoartritis of the hip
B. Bony metastasis from an occult malignancy
C. Multiple myeloma
D. Paget’s disease
E. Osteomalacia
Answer:
A young woman presents with a history of recurrent deep vein thrombosis presents with shortness of breath.
A 24-year-old nulliparous female with a history of recurrent deep vein thrombosis presents with shortness of breath.
The full blood count and clotting screen reveals the following results:
Hb 12.4 g/dl
Plateltes 137 WBC 7.5 * 109/l
PT 14 secs
APTT 46 secs
What is the most likely underlying diagnosis?
A. Third generation oral contraceptive pill use
B. Protein C deficiency
C. Antithrombin III deficiency
D. Antiphospholipid syndrome
E. Activated protein C resistance
Answer: D. Antiphospholipid syndrome
Discussion: The combination of a prolonged APTT and thrombocytopenia make antiphospholipid syndrome the most likely diagnosis.
Antiphospholipid syndrome
Antiphospholipid syndrome is an acquired disorder characterised by a predisposition to both venous and arterial thromboses, recurrent fetal loss and thrombocytopenia. It may occur as a primary disorder or secondary to other conditions, most commonly systemic lupus erythematosus (SLE) A key point for the exam is to appreciate that antiphospholipid syndrome causes a paradoxical rise in the APTT. This is due to an ex-vivo reaction of the lupus anticoagulant autoantibodies with phospholipids involved in the coagulation cascade
The full blood count and clotting screen reveals the following results:
Hb 12.4 g/dl
Plateltes 137 WBC 7.5 * 109/l
PT 14 secs
APTT 46 secs
What is the most likely underlying diagnosis?
A. Third generation oral contraceptive pill use
B. Protein C deficiency
C. Antithrombin III deficiency
D. Antiphospholipid syndrome
E. Activated protein C resistance
Answer: D. Antiphospholipid syndrome
Discussion: The combination of a prolonged APTT and thrombocytopenia make antiphospholipid syndrome the most likely diagnosis.
Antiphospholipid syndrome
Antiphospholipid syndrome is an acquired disorder characterised by a predisposition to both venous and arterial thromboses, recurrent fetal loss and thrombocytopenia. It may occur as a primary disorder or secondary to other conditions, most commonly systemic lupus erythematosus (SLE) A key point for the exam is to appreciate that antiphospholipid syndrome causes a paradoxical rise in the APTT. This is due to an ex-vivo reaction of the lupus anticoagulant autoantibodies with phospholipids involved in the coagulation cascade
Case regarding informing the patient or family first of any bad news...
What should you tell them?
a. You will honor their wishes.
b. You agree with their wishes and you ask them to give you the necessary written request.
c. You ask them to involve the ethics committee for the hospital.
d. You tell them that you are obligated to inform the patient of all the findings.
e. Explain to them that that decision can only be made y the health-care proxy.
Answer:
Regarding World Health Organization Roll Back Malaria plan
You are working with the public health minister of Malawi in a project to decrease malarial deaths in children younger than 5 years of age.
All of the following strategies are part of the World Health Organization Roll Back Malaria plan EXCEPT:
A. Artemisinin-based combination therapy
B. Early treatment with chloroquine alone
C. Indoor residual spraying
D. Insecticide-treated bed nets
E. Intermittent preventive treatment during pregnancy
Answer:
Treatment Of High BP in Pregnancy
A 32-year-old woman who is 22 weeks’ pregnant is admitted to the maternity ward and found to be hypertensive with a BP of 180/100 mmHg. This is her first pregnancy and it is otherwise uncomplicated. She has no other relevant medical history and her urinalysis is normal, as is renal and liver function.
Question
Which of the following should not be used to control her BP?
A Hydralazine
B Methyldopa
C Labetalol
D Ramipril
E Amlodipine
Answer:
Elevated blood pressure in the setting of acute ischemic stroke needs to be judiciously treated because:
A. High blood pressure needs to be treated aggressively in order to decrease the incidence of intracranial bleeding.
B. Acute elevations in blood pressure usually do not spontaneously decline.
C. Blood pressures above 160 mmHg systolic or 100 mmHg diastolic are immediately life-threatening.
D. Areas of ischemic brain lose autoregulation and may be dependent on elevated mean arterial pressure to maintain perfusion.
E. Aggressive lowering of blood pressure with acute ischemic stroke improves outcome.
Answer :
Saturday, July 15, 2017
Regarding the use of antiviral agents...
Select an antiviral agent for each patient.
a. Ganciclovir
b. Acyclovir
c. Interferon α
d. Didanosine
e. Ribavirin
f. Amantadine
g. Vidarabine
h. Zalcitabine
A military recruit develops pneumonia secondary to influenza A. Symptoms began 24 h prior to physician visit.
Answer: f. Amantadine
An HIV-positive patient with a CD4 count of 50 complains of the onset of visual blurring; opacity is seen on funduscopic exam.
Answer:a. Ganciclovir
A sexually active young woman has anogenital warts and requests intralesional therapy.
Answer: c. Interferon α
An infant with respiratory syncytial virus infection requires mechanical ventilation.
Answer: e. Ribavirin
Discussion:
Friday, July 14, 2017
A 66 year old woman presents with a history of weight loss - Case Study
History
A 66-year-old woman, a retired nurse, consults her general practitioner (GP) with a 4-month history of tiredness, slight breathlessness on exertion and loss of weight from 71 to 65 kg. Her appetite is unchanged and normal; she has no nausea or vomiting, but over the last 2 months she has had an altered bowel habit with constipation alternating with her usual and normal pattern. She has not seen any blood in her feces and has had no abdominal pain. She has had no post-menopausal bleeding. There is no relevant past or family history, and she is on no medication.
She has smoked 20 cigarettes daily for 48 years and drinks 20–28 units of alcohol a week.
Examination
She has slight pallor but otherwise looks well. No lymphadenopathy is detected, and her breasts, thyroid, heart, chest and abdomen, including rectal examination, are all normal.
The blood pressure is 148/90 mmHg.
Investigations:
- Haemoglobin = 10.1 g/dL (normal = 11.7–15.7 g/dL)
- Mean corpuscular volume (MCV) = 76 fL (normal = 80–99 fL)
- White cell count = 4.9 × 109/L (normal = 3.5–11.0 × 109/L)
- Platelets = 277 × 109/L (normal = 150–440 × 109/L)
- Sodium = 142 mmol/L (normal = 135–145 mmol/L)
- Potassium = 4.4 mmol/L (normal = 3.5–5.0 mmol/L)
- Urea = 5.2 mmol/L (normal = 2.5–6.7 mmol/L)
- Creatinine = 106 μmol/L (normal = 70–120 μmol/L)
- Urinalysis: no protein, no blood
- Blood film shows a microcytic hypochromic picture.
Questions
• What is the most likely diagnosis?
• How would you investigate the patient?
Case Discussion:
Post Coital Bleeding - Case Discussion
History
An 18-year-old woman is referred with postcoital bleeding. It has occurred on approximately seven occasions over the preceding 6 weeks. Generally it has been a small amount of bright red blood noticed a few hours after intercourse and lasting up to 2 days. There is no associated pain.
Her last menstrual period started 3 weeks ago and she bleeds for 4 days every 28 days. Her periods were previously quite heavy but are now lighter since she started the combined oral contraceptive pill (COCP) 6 months ago. There is no history of an abnormal discharge or offensive odour and she has no dyspareunia.
She has had three sexual partners and has been with her current partner for 10 months. She has never been diagnosed with any sexually transmitted infection and has never had a smear test. She had an appendectomy at the age of 7 years and was diagnosed with epilepsy in childhood but has been off all medication for 8 years.
Examination
The abdomen is soft and non-tender. Speculum examination reveals a florid reddened area symmetrically surrounding the external cervical os with contact bleeding. The uterus is normal sized, anteverted and non-tender. There is no cervical excitation and the adnexae are unremarkable.
Questions
• What is the differential diagnosis?
• What further investigations would you perform for this woman?
• If your investigations are negative what is the likely diagnosis and how would you manage the woman?
Case Discussion:
A patient presenting with fever and deranged LFTs ....
A 29-yr-old Catholic priest returns from a trip to Brazil with fevers and deranged LFTs. He has an ALT of 2500 U/l and bilirubin of 75 μmol/l. He attended a travel clinic and was vaccinated prior to travel. He also took mefloquine malaria prophylaxis.
What is the most likely diagnosis?
A. Malaria
B. Hepatitis A
C. Hepatitis B
D. Hepatitis E
E. Dengue fever
Answer:
Regarding Adverse Effects of Interferon - alpha...
A 36-year-old former intravenous drug user is to commence treatment for hepatitis C with interferon-alpha and ribavirin. Which of the following adverse effects are most likely to occur when patients are treated with interferon-alpha?
A. Diarrhoea and transient rise in ALT
B. Cough and haemolytic anaemia
C. Flu-like symptoms and transient rise in ALT
D. Haemolytic anaemia and flu-like symptoms
E. Depression and flu-like symptoms
Answer:
Regarding Disorders Of The Thyroid Gland...
Regarding Disorders Of The Thyroid Gland answer the following questions...
1. What are the key features in a patient's history that are important in assessing for a possible functional thyroid disorder?
2. What are the important physical examination findings?
3. What laboratory data are used to confirm or refute the existence of a functional thyroid abnormality?
Answers And Discussion
1. What are the key features in a patient's history that are important in assessing for a possible functional thyroid disorder?
When assessing a patient's history for clues to a functional thyroid disease, it is important to keep in mind that thyroid hormones in general control metabolism. Therefore, when questioning patients about their medical history, it is important to ask specifically about elements related to metabolism.
For example, in the setting of hyperthyroidism,
- weight loss,
- anxiety,
- tremor,
- palpitations,
- heat intolerance,
- hyperdefecation,
- insomnia,
- restlessness, and
- changes in the hair or skin are important features.
In contrast, in patients with suspected hypothyroidism, look for clues that indicate decreased metabolic activity. These include
Thursday, July 13, 2017
Tetralogy Of Fallot - Long Case Study
Presenting Complains:
- Breathlessness for … months
- Bluish discoloration of the lips and fingers during exertion for … months
- Weakness for … months
- Palpitation for … months
- Chest pain for … months
- Cough for … months.
History of Presenting Complains: According to the patient’s statement, she has been suffering from
breathlessness since her childhood. Her breathlessness was less marked in earlier stage, only felt
during moderate to severe activity. But for the last few months, it is progressively increasing, even
during mild exertion. There is no seasonal variation of breathlessness and it is not associated with
exposure to dust, pollen or fume. There is no history suggestive of paroxysmal nocturnal dyspnea or
orthopnea. The patient also noticed bluish discoloration of skin, finger nail, toes and lips for the last
… months, which is more marked during exercise and less by taking squatting position. She also
experiences diffuse chest pain, usually following any activity or after eating, which radiates to left
shoulder and subsides after taking rest. She also complains of palpitation, weakness and occasional
dry cough. Her bowel and bladder habits are normal. Her mother mentioned that the patient used to
become bluish and breathless while feeding or crying during the first few years of life.
On General Physical Examination:
- The patient is emaciated and short in stature
- Dyspneic
- Central cyanosis (involving tongue, lips, fingers and toes) is present
- There is generalized clubbing (involving all fingers and toes)
- Pulse: 112/min, low volume, regular in rhythm and normal character
- BP: 100/60 mm Hg
- Temperature: 98ºF
- Respiratory rate: 28/min
- No anemia, leukonychia, koilonychia, edema, jaundice, lymphadenopathy or thyromegaly
Cardiovascular system
- Pulse: 112/min, low volume, regular in rhythm and normal character
- BP: 100/60 mm Hg
- JVP: prominent “a” wave
- Visible cardiac impulse in apical and epigastric region
- Apex beat—palpable in the left … intercostal space, … cm from midline, normal in character
- Left parasternal lift and epigastric pulsation—present
- Systolic thrill—present in pulmonary area.
- First heart sound—normal in all the areas
- Second heart sound—P2 is soft (or absent) in pulmonary area, A2 is normal
- There is a harsh ejection systolic murmur in the pulmonary area, which radiates to the neck, more
on inspiration.
Examination of other systems reveals normal findings.
What is the Provisional Diagnosis?
Tetralogy Of Fallot (TOF)
Mention some cyanotic congenital heart disease.
As follows:
- Tricuspid atresia
- Transposition of great vessels
- Pulmonary atresia
- Ebstein’s anomaly.
What investigations are done in TOF?
As follows:
- Chest x-ray- shows boot-shaped heart, pulmonary conus is concave (small pulmonary artery), right ventricle enlarged (prominent elevated apex), oligemic lung, right-sided aortic arch in 25% cases.
- 2D echocardiography and color Doppler (diagnostic—it shows that the aorta is not continuous with the anterior ventricular septum).
- Other investigations: ECG (RVH), cardiac catheterization in some cases.
Wednesday, July 12, 2017
Anatomical Dead Space
The anatomical dead space may be used to calculate alveolar ventilation by subtracting it from the tidal volume and multiplying the result by the respiratory rate.
What would you expect the normal anatomical dead space to be in a healthy adult male?
A) 50 ml
B) 150 ml
C) 250 ml
D) 350 ml
E) 450 ml
Answer:
Transient Ischemic Attack
A 72-year-old woman with a past history of treated hypertension presents for review. Yesterday she had a 2 hour episode where she couldn't find the right word when speaking. This has never happened before and there were no associated features. Neurological examination is unremarkable and blood pressure was 150/100 mmHg. Her only current medication is amlodipine.
What is the most appropriate management?
A. Aspirin 300 mg immediately + specialist review within 2 weeks
B. Specialist review within 2 weeks
C. Aspirin 300 mg immediately + specialist review within 24 hours
D. Aspirin 75 mg + outpatient CT brain
E. Specialist review within 24 hours
Answer:
Tuesday, July 11, 2017
A woman with high BP reading recorded at her routine clinic visit...
A 71-year-old woman is reviewed in her local GP clinic. She has recently changed practices and is having a routine new patient medical. Her blood pressure is 146/94 mmHg. This is confirmed on a second reading. In line with recent NICE guidance, what is the most appropriate management?
A. Ask her to come back in 6 months for a blood pressure check
B. Arrange 3 blood pressure checks with the practice nurse over the next 2 weeks with medical review following
C. Arrange ambulatory blood pressure monitoring
D. Reassure her this is acceptable for her age
E. Start treatment with a calcium channel blocker
Answer:
Case Discussion - A Woman Presenting for Preconceptional Counseling ...
Mrs B, 24 years old had a previous baby with Down syndrome who is now one year old.She is desirous of further childbearing but is apprehensive about similar problem in the next baby and has come for preconceptional counseling. The karyotype of the affected child showed Trisomy 21 (47,XY).
Approach to the Case:
Points to be asked in History
• Age of the mother at delivery
• Period of gestation at which the pregnancy was registered
• First trimester scan for nuchal translucency
• Whether first or second trimester screening was done
• Second trimester anomaly scan
• Pregnancy outcome: Miscarriage, stillborn or live born
She mentions that her first pregnancy was a spontaneous conception. She sought antenatal care at 20 weeks of pregnancy. She had a term delivery at a hospital of a small for gestational age baby. The baby had mongoloid facies and a ventricular septal defect was diagnosed. The baby had delayed milestones and on investigations the baby was diagnosed with Trisomy 21.
What recurrence risk would you attribute to this lady?
Down’s syndrome cases result from nondisjunction, translocation or mosaic. With a pregnancy complicated by trisomy 21 from nondisjunction, the woman has 1% risk of having a pregnancy with trisomy in subsequent pregnancy. This risk pertains unless her age related risk exceeds it. Because of this risk, she would be offered invasive prenatal diagnosis. Parental karyotype is not indicated in this
couple.
What is the incidence of Down syndrome in general population?
Down’s syndrome occurs in 1 in 800 to 1 in 1000 newborns
Regarding Benzodiazepine Toxicity ..
A 24-year-old woman is brought to the emergency department with confusion, blurred vision, dizziness, and somnolence. Her friend states that the woman is generally healthy but is taking medication for occasional episodes of intense fear, sweating, nausea, and abdominal and chest pain. Physical examination reveals a respiratory rate of 8/min.
What is the most likely diagnosis?
Benzodiazepine toxicity, as characterized by respiratory depression, confusion, and other symptoms of central nervous system depression.
What class of drugs might be responsible for this patient’s symptoms?
Her friend’s description is consistent with a diagnosis of panic disorder. Benzodiazepines (such as
clonazepam, lorazepam, and alprazolam) are commonly used in the short-term treatment of panic disorder.
What treatment was likely administered to this patient in the emergency department?
Flumazenil, a competitive antagonist at the γ-aminobutyric acid (GABA) receptor, is effective in reversing symptoms of benzodiazepine overdose.
Haemochromatosis - Quick Case Discussion
Haemochromatosis
This 52‐year‐old man was referred after a diagnosis of diabetes mellitus was made by his GP. Please
examine him and discuss further investigations.
Clinical signs
• Increased skin pigmentation (slate‐grey colour)
• Stigmata of chronic liver disease
• Hepatomegaly
Scars of
• Venesection
• Liver biopsy
• Joint replacement
• Abdominal rooftop incision (hemihepatectomy for hepatocellular carcinoma)
Evidence of complications
• Endocrine: ‘bronze diabetes’ (e.g. injection sites), hypogonadism and testicular atrophy
• Cardiac: congestive cardiac failure
• Joints: arthropathy (pseudo‐gout)
Discussion
Sunday, July 9, 2017
A 70 year old man in the surgical ward 24 hours after a colon resection...
Twenty-four hours after colon resection, urine output in a 70-year-old man is 10 mL/h.
Blood chemistry analysis reveals sodium, 138 mEq/L; potassium, 6 mEq/L; chloride, 100 mEq/L; bicarbonate, 14 mEq/L.
His metabolic abnormality is characterized by which of the following?
(A) Abdominal distension
(B) Peaked T waves
(C) Narrow QRS complex
(D) Cardiac arrest in systole
(E) J wave or Osborne wave
Answer:
Regarding child's developmental milestones...
An infant can regard his parent’s face, follow to midline, lift his head from the examining table, smile spontaneously, and respond to a bell. He does not yet regard his own hand, follow past midline, nor lift his head to a 45° angle off the examining table.
Which of the following is the most likely age of the infant?
a. 1 month
b. 3 months
c. 6 months
d. 9 months
e. 12 months
Answer:
Regarding School exclusion advice
Regarding School exclusion advice
A. Five days from onset of rash
B. Five days from onset of swollen glands
C. Five days from commencing antibiotics
D. Until symptoms have settled for 48 hours
E. Until lesions have crusted over
F. Until treated
G. No exclusion
H. Until symptoms have settled for 12 hours
For each one of the following infectious diseases, select the most appropriate advice regarding school exclusion:
Whooping cough
Answer: C. Five days from commencing antibiotics
Roseola
Answer: G. No exclusion
Diarrhea and vomiting
Answer: D. Until symptoms have settled for 48 hours
Discussion: Below is summarized Health Protection Agency guidance on school exclusion:
Case Discussion - Cardiac Failure Developing On 3rd day Postpartum
A 27 year old female para 2 (h/o of both LSCSs), on the 3rd postoperative day of caesarean develops sudden cardiac failure.
– She has weakness, shortness of breath, palpitation, nocturnal dyspnea and cough.
– O/E- Tachycardia, arrhythmia, peripheral edema, pulmonary rales are present. S3 is present but no murmur is heard.
– She had been a booked patient with regular antenatal checkups and with no prior heart problem and uneventful prior obstetric history.
What is the probable diagnosis?
Case Discussion:
The diagnosis of peripartum cardiomyopathy should be kept in mind in all such cases.
The criteria for diagnosis are:
1. Cardiac failure within last month of pregnancy or within 5 month postpartum.
2. No determinable cause for failure (may be immunological or nutritional).
3. No previous heart disease.
4. Left ventricular dysfunction (Echocardiography) as evidenced by ejection fraction < 45%
5. Left ventricular end-diastolic dimension > 2.7 cm/m2.
Regarding Pacemaker Function...
A 72-year-old woman had a pacemaker inserted 4 years ago for symptomatic bradycardia because of AV nodal disease. She is clinically feeling well and her ECG shows normal sinus rhythm at a rate of 68/min but no pacemaker spikes. Her pacemaker only functions when the ventricular rate falls below a preset interval.
Which of the following best describes her pacemaker function?
(A) asynchronous
(B) atrial synchronous
(C) ventricular synchronous
(D) ventricular inhibited
(E) atrial sequential
Answer: (D) ventricular inhibited
Discussion: The ventricular inhibited (VVI) pacemaker functions when the heart rate falls below a preset interval. If a QRS is detected, the pacemaker is inhibited. If a QRS is not sensed, the pacing stimulus is not inhibited and the ventricle is stimulated
A 14-year-old boy comes to the office because his breasts have recently become tender and slightly swollen...
A 14-year-old boy comes to the office because his breasts have recently become tender and slightly
swollen. He is worried that he is undergoing feminization and will grow up to become a “freak.” Upon examination a tender, 2-cm mass is found to be palpable in the subareolar region of both breasts. Which of the following describes the best course of action?
(A) Excise the masses by performing a subcutaneous mastectomy.
(B) Incise and drain the masses.
(C) Treat the masses with topical steroids.
(D) Aspirate the masses for culture and cytology.
(E) Leave the masses alone.
Answer:
Regarding chromosomal aberrations in spontaneous miscarriages...
A 24-year-old woman has had three first-trimester spontaneous miscarriages.
Which of the following statements concerning chromosomal aberrations in miscarriages is true?
a. 45,X is more prevalent in chromosomally abnormal term babies than in abortus products
b. Approximately 20% of first-trimester spontaneous abortions have chromosomal abnormalities
c. Trisomy 21 is the most common trisomy in abortuses
d. Despite the relatively high frequency of Down syndrome at term, most Down fetuses abort spontaneously
e. Stillbirths have twice the incidence of chromosomal abnormalities as live births
Answer:
Diabetes mellitus: Management of type 2..
A 64-year-old man is reviewed in clinic. He has a history of ischemic heart disease and was diagnosed with type 2 diabetes mellitus around 12 months ago. At this time of diagnosis his HbA1c was 7.6% (60 mmol/mol) and he was started on metformin which was titrated up to a dose of 1g bd. The most recent bloods show a HbA1c of 6.8% (51 mmol/mol). He has just retired from working in the IT industry and his body mass index (BMI) today is 28 kg/m2.
His other medication is as follows: Atorvastatin 80mg od, Aspirin 75mg od, Bisoprolol 2.5 mg od, Ramipril 5mg od .
What is the most appropriate next step?
A. Add sitagliptin
B. Make no changes to his medication
C. Add glimepiride
D. Add pioglitazone
E. Add exenatide
Answer:
Management of Hyponatremia..
Five days after an uneventful cholecystectomy, an asymptomatic middle-aged woman is found to have a serum sodium level of 120 meq/L.
Proper management would be
a. Administration of hypertonic saline solution
b. Restriction of free water
c. Plasma ultrafiltration
d. Hemodialysis
e. Aggressive diuresis with furosemide
Answer:
Saturday, July 8, 2017
Regarding Gravidity and Parity...
Regarding Gravidity and Parity...
A G1 P0
B G4 P2
C G0 P0
D G3 P3
E G2 P1
F G1 P2
G G6 P0
H G5 P2
I G1 P1
J G3 P1
K G4 P3
L G2 P0
For each description below, choose the SINGLE most appropriate answer from the above list of options. Each option may be used once, more than once, or not at all.
1 A woman currently pregnant who has had a previous term delivery.
2 A woman not currently pregnant who has had one previous termination, one early miscarriage and one stillbirth at 36/40.
3 A woman who attends for pre-conception counselling, never having been pregnant.
4 A woman currently pregnant with twins who has had one previous early miscarriage.
5 A woman not currently pregnant who previously had a twin delivery at 28/40.
Answers:
A 65-year-old male presents with arthralgia and sleep disturbance following the introduction of simvastatin...
A 65-year-old male presents with arthralgia and sleep disturbance following the introduction of simvastatin. He has a history of hypertension and ischemic heart disease for which he is receiving aspirin, atenolol and eprosartan together with simvastatin 40 mg once daily, which has been introduced in the last one month. Previously, he had been taking atorvastatin but this was changed to simvastatin after he complained of arthralgia.
Investigations reveal:
Creatine Phosphokinase (CPK) 156 iu/l (40-170)
Total Cholesterol 5.1 mmol/l (<5.2)
LDL-Cholesterol 3.1 mmol/l (<2.6)
Triglycerides 1.7 mmol/l (0.5-1.7)
HDL-Cholesterol 1.2 mmol/l (0.7-1.7)
Which is the most appropriate treatment for his lipid profile?
A- Ezetimibe
B- Fenofibrate
C- Nicotinic acid slow release
D- Omega-3 fatty acids
E- Rosuvastatin
Answer:
Subscribe to:
Comments (Atom)