A blog designed to help medical students and doctors preparing for undergraduate and postgraduate exams
Wednesday, February 15, 2017
A Patient presents With Acute Abdominal Pain Secondary To Renal stones....
A 34-year-old man presents to an emergency surgery with abdominal pain. This started earlier on in the day and is getting progressively worse. The pain is located on his left flank and radiates down into his groin. He has had no similar pain previously and is normally fit and well. Examination reveals a man who is flushed and sweaty but is otherwise unremarkable.
What is the most suitable initial management?
A. Oral ciprofloxacin
B. IM diclofenac 75 mg
C. Oral co-amoxiclav and metronidazole
D. IM morphine 5 mg
E. IM diclofenac 75 mg + start bendroflumethiazide to prevent further episodes
Answer:
Treatment After Being Bitten By Pet Dog...
A 40-yr-old man presents with a swollen erythematous finger and right axillary tenderness, 24 hours after being bitten by his pet dog. What is the best Rx?
A. Metronidazole
B. Aciclovir
C. Fluconazole
D. Flucloxacillin
E. Co-amoxiclav
Answer:
Regarding Lung Cancer....
A 65-yr -old woman has been diagnosed as having lung cancer. Which of the following statements is most appropriate?
A. Hypertrophic pulmonary osteoarthropathy (HPOA) is commonly seen pts with small-cell
carcinoma
B. SIADH is commonly seen in pts with squamous-cell carcinoma
C. Hypercalcaemia may occur without bone metastasis
D. Paraneoplastic syndromes occur more commonly with squamous-cell carcinomas
E. Hypercalcaemia associated with bone metastasis is best treated with intravenous steroids
Answer:
Monday, February 13, 2017
A 54 Year Old Man With Epilepsy And Ischemic Heart Disease Presents With Complains Of Lethargy
A 54-year-old man with a history of epilepsy and ischaemic heart disease is seen in clinic with a 3 month history of lethargy.
Blood tests are as follows:
Hb 9.6 g/dl
MCV 123 fl
Plt 164 * 109/l
WCC 4.6 *109/l
Which one of his medications is most likely to be responsible?
A. Clopidogrel
B. Atorvastatin
C. Carbamazepine
D. Atenolol
E. Phenytoin
Answer:
Blood tests are as follows:
Hb 9.6 g/dl
MCV 123 fl
Plt 164 * 109/l
WCC 4.6 *109/l
Which one of his medications is most likely to be responsible?
A. Clopidogrel
B. Atorvastatin
C. Carbamazepine
D. Atenolol
E. Phenytoin
Answer:
Appropriate Management For A Patient With Advanced Cancer Who Presents With Tearful And Upset Behavior.
Appropriate Management For A Patient With Advanced Cancer Who Presents With Tearful And Upset Behavior.
Lung Abscess - Long Case With Questions & Answers
Chief complaints:
- Cough with profuse foul smelling sputum for … days
- Hemoptysis for … days
- Fever for … days
- Chest pain for … days
- Malaise, weakness, loss of weight for … days.
History of present illness: According to the statement of the patient, he was reasonably well … days
back. Since then, he has been suffering from severe cough with production of copious foul smelling
purulent sputum. It is occasionally associated with scanty amount of blood. He also complains of
high grade continuous fever, highest recorded 104°F. The fever is associated with chills and rigors
and profuse sweating, subsides only with paracetamol. The patient also complains of right sided chest
pain, which is compressive in nature, worse with inspiration and during coughing, but there is no
radiation. For the last ... days, he is also suffering from malaise, weakness, anorexia and loss of
approximately 15 kg of body weight. His bowel and bladder habits are normal.
History of past illness: He was suffering from pneumonia 6 months back from which there is complete recovery.
Family history: Nothing significant.
Personal history: He smokes about 25 sticks a day for 25 years. He is also an alcoholic.
Socioeconomic history: He is a day laborer and lives in a slum area with poor sanitation.
Drug history: The patient was treated by local physicians with antibiotics, cough syrup and
paracetamol, but no improvement.
General Examination
The patient looks toxic and emaciated
Generalized clubbing is present in all the fingers and toes
Moderately anemic
No jaundice, cyanosis, koilonychia, leukonychia or edema
No thyromegaly or lymphadenopathy
Vitals:
Pulse: 110/min
BP: 110/75 mm Hg
Temperature: 103º F
Respiratory rate: 28/min.
Systemic Examination
Respiratory System: (Supposing right sided)
Inspection:
- Movement is restricted in the right side of the chest.
Palpation:
- Trachea is central in position
- Apex beat is in the left 5th intercostal space in the midclavicular line
- Vocal fremitus is increased on the right side of the chest
- Chest expansion is reduced on the right side.
Percussion:
- Percussion note is woody dull over right side of chest from … to … intercostal space
- Upper border of the liver dullness is in the right 5th intercostal space in midclavicular line
- Cardiac dullness is normal.
Auscultation:
- Breath sound is bronchial in … intercostal space on the right side. In other places, it is vesicular.
- Vocal resonance is increased over the same area
- There are coarse crepitations over the right side of the chest in … intercostal space, reduces on coughing.
Examination of the other systems reveals no abnormalities.
Provisional diagnosis: Right sided Lung Abscess.
Questions Likely To Be Asked By The Examiner:
Q. What are the differential diagnoses?
A. As follows:
- Consolidation (during resolution stage)
- Bronchiectasis
- Bronchial carcinoma
- Pulmonary TB.
Regarding Side Effects Of Aminosalicylate Drugs Like Mesalazine (Used In treatment of Ulcerative Colitis)
A 36-year-old man is reviewed in clinic. He has recently been started on mesalazine 400mg tds for ulcerative colitis. Which one of the following adverse effects is least likely to be attributable to mesalazine?
A. Interstitial nephritis
B. Headaches
C. Acute pancreatitis
D. Agranulocytosis
E. Infertility
Answer:
Sudden Cardiac Death
Regarding Sudden Cardiac Death answer the following questions:
1. What kind of heart disease is seen most commonly in adults who die suddenly? In young athletes?
2. Which types of arrhythmias are associated with cardiac arrest and sudden cardiac death (SCD)?
3. Which patients are at highest risk for SCD?
4. What is the cause of SCD in the long QT syndrome?
Answers:
1. What kind of heart disease is seen most commonly in adults who die suddenly? In young athletes?
Approximately 90% of cases of SCD are due to ventricular fibrillation in the setting of preexisting structural heart disease; 5% to 10% occur in the absence of organic heart disease.
In individuals younger than 30 years and young athletes, SCD is very rare, but when it does occur it is usually due to hypertrophic cardiomyopathy. Arrhythmogenic right ventricular dysplasia and
acute myocarditis are other infrequent causes of SCD in the young adult.
After the age of 40, 65% to 70% of all SCDs are attributable to Coronary artery disease.
2. Which types of arrhythmias are associated with cardiac arrest and SCD?
In the field, paramedics most commonly record ventricular fibrillation or ventricular tachycardia during cardiac arrest. Less frequently seen, and associated w ith a poorer prognosis, are
Saturday, February 11, 2017
Treatment For A Suspected Case Of Tuberculous Meningitis
A 40-yr-old woman presents with progressive confusion and mild neck stiffness. She has
suffered from increasing headaches over the past 4-6 wks, and over the past wk she has begun
to suffer from worsening drowsiness and confusion, with neck stiffness. A CT scan showed basal
meningeal enhancement. A lumbar puncture showed an opening pressure of 200 mmH2O, a
turbid CSF with 500 leucocytes/ml (90% lymphocytes), a glucose concentration of 1 mmol/l and
negative results with Gram, Indian ink and Ziehl–Neelsen stains. CSF protein is elevated at
1.05g/l (<0.50).
What is the best Rx?
A. Rifampicin + INAH + pyrazinamide + Ethambutol
B. Ceftriaxone
C. Aciclovir
D. Corticosteroids
E. Liposomal amphotericin B
Answer:
Friday, February 10, 2017
Regarding “Pneumonia” Vaccine....
A. High-risk infants should receive the 23-valent pneumococcal vaccine.
B. Heptavalent pneumococcal vaccine alone is recommended for high-risk children older than age 2 years.
C. Children with sickle cell disease or asplenia who receive the pneumococcal vaccine still require antibiotic prophylaxis.
D. Pneumococcal vaccine is not recommended for healthy infants.
E. Pneumococcal vaccine may not be administered at the same time as MMR, varicella, or poliovirus vaccines.
Answer :
D. Pneumococcal vaccine is not recommended for healthy infants.
E. Pneumococcal vaccine may not be administered at the same time as MMR, varicella, or poliovirus vaccines.
Answer :
Regarding Alzheimer's disease...
A 69-year-old man who is known to have Alzheimer's disease is reviewed in clinic. His latest Mini Mental State Examination (MMSE) score is 18 out of 30.
According to NICE guidelines, what further action should be taken?
A. Supportive care + memantine
B. Supportive care + trial of citalopram
C. Continue supportive care
D. Supportive care + donepezil + low-dose aspirin
E. Supportive care + donepezil
Answer:
Prostate Cancer: Management
A 72-year-old man is diagnosed with prostate cancer and goserelin (Zoladex) is prescribed. Which one of the following is it most important to co-prescribe for the first three weeks of treatment?
A. Tamoxifen
B. Lansoprazole
C. Allopurinol
D. Cyproterone acetate
E. Tamsulosin
Answer:
Thursday, February 9, 2017
A 57 year Old Man With Hypertension And History Of Smoking Presents With Complains Of Pressure Like Sensation In His Chest.
A 57-year-old automobile salesman who is hypertensive and a heavy cigarette smoker describes a pressure-like sensation that developed for the first time 3 weeks before. The discomfort, which begins in the retrosternal area, radiates to the left side of his lower jaw, occurs when he walks rapidly in cold air, and more recently occurs at rest.
Careful history reveals that it lasts for 10 to 15 minutes, but an especially severe episode awakened him the night before and lasted nearly half an hour before resolving spontaneously.
Except for a bloodpressure of 150/100 mm Hg, the physical examination findings are normal.
An ECG (obtained after the pain has disappeared) reveals deep and symmetric T wave inversion in leads V1 to V4. The patient is admitted and given IV heparin and oral aspirin.
1. What is your diagnosis?
2. What are some common physical findings during an ischemic episode?
Approximately 4 hours after admission, the patient again experiences transient chest pressure. You order an ECG. The T waves are now upright in leads V1 to V4.
3. What are these ECG changes called, and what do they represent?
4. How should the recurrent chest pain be treated?
5. What should be done next?
Answers:
Celiac disease - Investigations
A 26-year-old woman who is known to have type 1 diabetes mellitus presents with a three-month history of diarrhoea, fatigue and weight loss. She has tried excluding gluten from her diet for the past 4 weeks and feels much better. She requests to be tested so that a diagnosis of coeliac disease is confirmed.
What is the most appropriate next step?
A. Check her HbA1c
B. No need for further investigation as the clinical response is diagnostic
C. Check anti-endomysial antibodies
D. Arrange a jejunal biopsy
E. Ask her to reintroduce gluten for the next 6 weeks before further testing
Answer:
Tuesday, February 7, 2017
Marker Of Prognosis In Paracetamol Overdose
A 17-year-old girl presented with jaundice three days after having taken a paracetamol and alcohol overdose during an argument with her boyfriend.
What is the best marker of prognosis?
a. Serum aspartase transaminase.
b. Serum alkaline phosphatase.
c. Serum bilirubin.
d. Prothrombin time.
e. Paracetamol level.
Answer:
Radiologic Study Important In The Diagnosis Of Posterior Shoulder Dislocations?
A. True AP view
B. Transcapular lateral view
C. Axillary lateral view
D. Scapular Y view
E. Serendipity view
Answer :
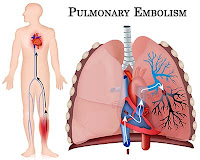
Clinical Features In A Patient With Pulmonary Embolism
A 64-yr -old woman is referred to the medical team from the orthopaedic ward. She underwent a right total hip replacement 6 days ago. She is known to suffer from mild chronic obstructive pulmonary disease and is on regular inhaled steroids and a short-acting β2-agonist.
She now complains of left-sided chest pain and is also dyspnoeic.
Your clinical Dx is pulmonary embolism.
Which one of the following would not be a feature of pulmonary embolism in this pt?
A. Dyspnoea
B. Tachypnoea
C. New-onset atrial fibrillation
D. Fever
E. Bradycardia
Answer:
Differentiating A Panic Disorder From Generalized Anxiety Disorder
Regarding differentiating a Panic disorder from Generalized Anxiety disorder answer the following question:
Answer And Discussion:
Pleural Effusion - Long Case With Questions And Answers
Case History
Presenting Complaints:
- Cough with slight expectoration for … weeks
- Breathlessness for … days
- Fever for … days
- Weight loss for … days.
History Of Presenting Complaints: According to the statement of the patient, he was alright … weeks back. Since then, he has been suffering from frequent cough, which is present throughout day and night. The cough is usually dry with occasional slight expectoration of mucoid sputum, but no hemoptysis. He is also complaining of breathlessness, which is more marked during moderate to severe exertion, but there is no history of orthopnea or paroxysmal nocturnal dyspnea. The patient also complains of low grade continued fever for … days, more marked in the evening and associated with night sweats. During this period, he lost about 15 kg of body weight. There is no history of chest pain, joint pain or swelling, skin rash or any contact with patient with pulmonary TB. His bowel and bladder habits are normal.
General Physical Examination:
- The patient is ill-looking and emaciated
- Mildly anemic
- No jaundice, cyanosis, clubbing, edema, koilonychia or leukonychia
- No lymphadenopathy or thyromegaly
Vitals:
- Pulse: 100/min
- BP: 130/75 mm Hg
- Temperature: 100º F
- Respiratory rate: 24/min.
Respiratory system: (supposing right sided effusion)
Inspection:
Movement is restricted on lower part of right side of the chest with fullness of intercostal spaces
(Mention, if any puncture mark, gauze and tape indicating aspiration of pleural fluid).
Palpation:
Trachea is shifted to the left side
Apex is shifted to the left (in 6th intercostal space in the anterior axillary line), normal in character
Vocal fremitus is reduced in right lower chest up to … ICS (tell where)
Chest expansion is restricted over the right lower chest.
Percussion:
There is stony dullness in the right lower chest up to … ICS (tell where).
Auscultation:
Breath sound—diminished (or absent) in the right lower chest
Vocal resonance—diminished (or absent) in the right lower part of chest
No added sound.
Note: Just above the upper level of effusion, the following findings may be present (mention, if any)
¯¯ Bronchial sound
¯¯ Increased vocal resonance
¯¯ Whispering pectoriloquy
¯¯ Pleural rub.
Examination of the other systems reveals no abnormalities.
Provisional Diagnosis: My diagnosis is right sided pleural effusion.
Questions Likely To Be Asked By The Examiner:
Sunday, February 5, 2017
Regarding Dermatomes.....
A 55-year-old woman complains of neck and right arm pain for the past two months. The pain is often triggered by flexing her neck. Her past medical history includes osteoarthritis of her knee, obesity and depression.
On examination there is no obvious muscle atrophy or weakness of the right arm. There is however some sensory loss over the middle finger and palm of the hand.
Which nerve root is most likely to be affected by the impingement?
A. C4
B. C5
C. C6
D. C7
E. C8
Answer:
Saturday, February 4, 2017
Normal Physiologic Changes With Aging
A. Decrease in creatinine clearance
B. Blood pressure of 160/80
C. Elevated FEV1 value on pulmonary function tests
D. Low-frequency hearing loss
E. Maximum stress test heart rate of 90
Answer :
Thursday, February 2, 2017
Case Study Of A 20-year-old woman with no significant past medical history presents with a 2-month history of episodic shortness of breath.
A 20-year-old woman with no significant past medical history presents with a 2-month history of episodic shortness of breath. These symptoms began with an upper respiratory tract infection. She has fits of coughing and trouble catching her breath with exertion. She states that her breath “sounds like whistles” at times. She tried a friend’s albuterol inhaler with some improvement and wonders if she has asthma. On exam, she is breathing comfortably at 16 times per minute and her oxygen saturation is 96% on room air. Her lungs are clear to auscultation, and the remainder of her exam is unremarkable. You want to better categorize, this patient’s disease.
Which of the following tests is most appropriate to order now?
A) Spirometry.
B) Chest x-ray.
C) Arterial blood gas (ABG).
D) Methacholine challenge.
E) Chest CT.
Answer And Discussion
The correct answer is “A.” Spirometry.
Since this patient has symptoms of bronchospasm, spirometry will be essential in determining if there is objective evidence of obstructive lung disease. However, spirometry results are often normal in mild cases of asthma, especially when the patient is asymptomatic. Bronchoprovocation testing, with methacholine or histamine, may be useful in such cases, but should follow basic spirometry. Although chest radiography (x-ray or CT) may reveal an unsuspected process, it is not indicated in
otherwise healthy patients with symptoms of bronchospasm.
Bacterial pneumonia is a potential precipitant of bronchospasm that may be diagnosed on chest x-ray, but this patient has no constitutional symptoms (like fever) associated with serious bacterial infection. ABG levels may be helpful when a patient presents with respiratory distress but certainly not in the office setting.
If this patient has mild asthma, which of the following pulmonary function test results would you expect to find?
A) Forced vital capacity (FVC) 50% of predicted.
B) Forced expiratory volume in 1 second (FEV1)
100% of predicted.
C) FEV1/FVC ratio <0.7.
D) Total lung capacity (TLC) 50% of predicted.
E) FEV1/TLC <0.7.
Answer And Discussion
Wednesday, February 1, 2017
Tests Done In The Diagnosis Of Helicobacter pylori Infection
A 54-year-old man is investigated for dyspepsia. An endoscopy shows a gastric ulcer and a CLO test (rapid urease test) done during the procedure demonstrates H. pylori infection. A course of H. pylori eradication therapy is given. Six weeks after completing treatment the patients comes for review. Unfortunately his symptoms have not improved. What is the most appropriate test to confirm H. pylori eradication?
A. Culture of gastric biopsy
B. H. pylori serology
C. Hydrogen breath test
D. Urea breath test
E. Stool culture
Answer:
Sarcoidosis- Diagnosis
A 35-yr -old woman complains of a painful rash on her legs. She also gives a three-mth history
of dyspnoea on exertion. Her doctor arranged for her to have a CXR and this shows bilateral hilar
prominence. Examination of her legs reveals a purplish-red, nodular tender rash on her shins.
Apart from few bi-basal crepitations on auscultation, systemic examination is normal. A
pulmonary function test shows a mildly impaired DLCO. Which one of the following is the best
investigation to confirm the Dx?
A. Sputum microscopy and culture
B. High-resolution CT scan of the thorax
C. Open lung biopsy
D. Kveim test
E. Serum ACE level
Answer: B) High-resolution CT scan of the thorax
Discussion: This woman has erythema nodosum and bilateral hilar lymphadenopathy. This suggests that she has sarcoidosis. This has a good prognosis.
A 42 Year Old Woman with History Of Diabetes Presents With Chest Pain - Case Study
A 42-year-old registered nurse is seen because of pain in the chest. She describes a “pain in my heart” and points to a 1-cm area above the left breast. The pain is intensified by deep breathing, coughing, recumbency, and twisting motions. It has lasted continuously for 2 days. Three days ago, she noted extreme fatigue and shortness of breath lasting for 24 hours. Findings from a complete physical examination are normal.
1. What is the most likely diagnosis in this patient, and why?
As you are about to discharge this patient, her husband tells you he is concerned about his wife because her sister underwent coronary bypass surgery at 44 years and her brother at 34 years. Because the pain has some features of pericarditis, you decide to do an ECG. It shows normal sinus rhythm with Q waves in the inferior leads and diffuse ST-segment elevation.
2. What is your diagnosis, and w hat would you do?
Answers:
Subscribe to:
Posts (Atom)